The Flying Flu: Avian Influenza & Virus Surveillance
In this Thoughts On... post, we discuss the recent avian influenza outbreak, beginning with details on influenza virus biology and ending with current efforts in management and viral surveillance.
Introduction
Over the past few months, you may have seen headlines about the resurgence of a virus found around the world, including in different parts of the continental United States. This virus, an avian influenza, is also known as bird flu, highly pathogenic avian influenza (HPAI), or by its subtype (H5N1). According to the Centers for Disease Control and Prevention (CDC), as of the publishing date of this piece, there have been twenty-seven human cases of avian influenza in the United States. These individuals acquired the virus from interactions with infected cows or poultry present on farms. In this issue, we’ll provide some general information about influenza viruses and discuss the cases in birds, cows, and humans that have appeared across the United States within this current avian influenza outbreak. Then, we will discuss the importance of flu vaccination and viral surveillance, drawing on efforts made by government and research entities to monitor and control the spread of avian influenza.
Background: What Does H5N1 Mean?
Viruses are nonliving particles made up of protein and nucleic acid (DNA or RNA), and depending on the kind of virus, lipids. On their surface, they are decorated with viral surface proteins. There is a chance you may have heard the word “spike” thrown around in articles or news pieces about COVID-19. This refers to the surface proteins sticking out of SARS-CoV-2, the virus that causes COVID-19. These proteins touch and bind certain proteins on the surface of human cells; this point of contact with the cell is the first step in the process of viral entry into cells. Influenza viruses have their own kind of surface proteins that they use to enter and exit host cells. These surface proteins are referred to as hemagglutinin (HA) and neuraminidase (NA), giving rise to the H_N_ nomenclature of influenza viruses.

So, we have H (hemagglutinin) and N (neuraminidase), but where do the numbers come from? There are many different subtypes of these proteins–eighteen different HAs and eleven NAs, to be exact. The subtypes are a minimum of 30% different from one another, and an influenza virus can have any combination of HA and NA on its surface, giving rise to all the different variations we see.

Influenza viruses can infect a wide range of animals, from birds to pigs, seals to horses, and as anyone who’s stayed home sick with the flu can tell you, humans too. But what determines who gets infected? Here’s where those HA and NA surface proteins come into play. Hemagglutinin (HA), with all its different subtypes, preferentially binds host cell molecules of certain species. For example, HA binds to a certain sugar called sialic acid (SA) present on the surface of cells, but sialic acid can look different in different animals. Birds have a slightly different arrangement of the atomic bonds in sialic acid than humans, meaning some influenzas that contain H10, the 10th subtype of hemagglutinin, mostly infect birds, while H1, 2, and 3 can infect humans. However, this becomes more complicated when we bring pigs into the mix. Pigs have both types of sialic acid, meaning a pig can be infected with an influenza virus that primarily infects birds and another one that infects humans at the same time. Viruses are tricky to manage due to the fact that they can undergo what we call genetic reassortment, allowing them to rapidly evolve. Basically, the HA’s and NA’s can “shuffle”, giving rise to new combinations inside pigs. These reassorted viruses can be passed to humans and become more infectious or transmissible, leading to epidemics and pandemics such as the H1N1 influenza pandemic strain that circulated throughout the world in 2009, referred to commonly as “swine flu”.
Spilling Over
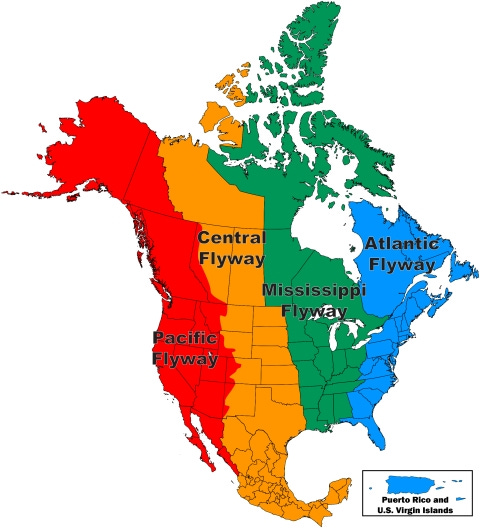
Avian influenza mainly circulates in birds, meaning it can travel very long distances as birds migrate and cross paths, encountering other species. If we look at where several of the human cases have emerged in the United States (Texas, Colorado, California), we see that they lie within the Central and Pacific Flyways, common paths that migrating birds take between nesting and wintering locations.
The human cases of avian influenza H5N1 we have seen this year are the result of what is referred to as a spillover event, when viruses predominantly infecting one species jump and infect another species. In the case of dairy farm workers who became infected across the United States, this likely occurred from the avian influenza spilling over and replicating in dairy cows, and then spilling over and infecting the workers. However, because H5N1 is not adapted to transmit human-to-human, we are not seeing a large boom in cases—so far. This doesn’t mean the virus is not a problem, though, since the H5N1 influenza virus has been shown to be lethal in some cases. Continued infection in bird populations coupled with vast avian migratory patterns means we will continue to see spillover into other animals, including humans.
I’m Not a Farmer, How Does This Affect Me?
If you don’t work on a poultry or dairy farm, or regularly come into contact with sick birds, you shouldn’t worry about contracting H5N1 now. The World Health Organization (WHO) releases regular risk assessments for humans, and the CDC is actively monitoring circulating strains and human infections in the event that H5N1 begins spreading from human-to-human. That being said, there are some precautions you can take. For starters, limit exposure to sick or dead animals, including but not limited to birds, and their feces. Cook animal products such as eggs and meat to safe internal temperatures (165ºF for chicken, 145ºF for beef and pork) to kill pathogens, and avoid unpasteurized (raw) milk. Pasteurization is necessary to kill microbes including influenza viruses, and raw milk may be at risk of containing harmful pathogens that can cause serious disease.
Another critical measure for protecting against general influenza infection is getting a yearly flu vaccine. It’s important to note that efforts to make a vaccine against avian influenza often prove difficult due to the rapid viral mutation rate as this virus is rapidly transmitted around the world. A vaccine made against the current avian flu strain may not be as effective for future strains that may pose more harm to humans. In terms of vaccination against the common human influenza viruses, not every human-infecting strain is circulating with the same frequency at all times. With so many HA’s and NA’s and the accumulation of mutations over time, there is a seemingly endless variety of possibilities. Each year, a decision is made on what the composition of that year’s flu vaccine will be, informed by global epidemiological surveillance of flu circulation in different areas, genetic information on virus mutations and different strains, how our immune systems recognize circulating viruses, and a whole host of other important studies. This means that flu vaccines are a little different each year, so if you got a vaccine three years ago you likely will not be up to date on the current influenza viruses that will be circulating this year. This all goes to say, make sure to stay up to date with your flu vaccines!
Current State of Surveillance (Or, The Lack Thereof…)
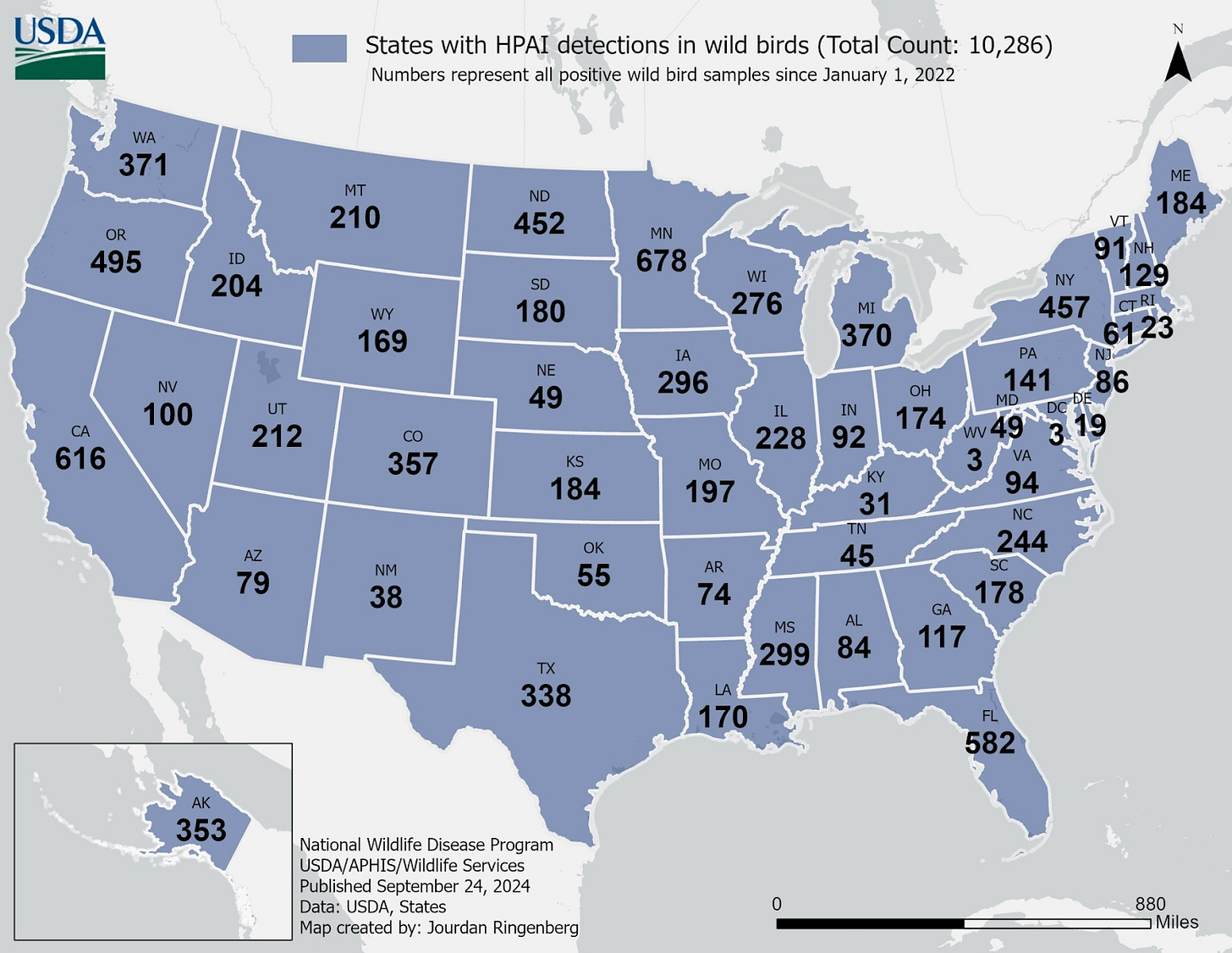
Human cases continue to pop up throughout the continental United States, from Texas to Michigan and, lately, California. Fourteen states have reported outbreaks of H5N1 influenza in dairy cows, with spillover into humans occurring periodically. Since human infections seem to be unpredictable and crop up across several states, monitoring in people is difficult, but that doesn’t mean that more cannot be done in animal disease surveillance. Currently, the USDA is testing raw milk for the virus, and the FDA is testing commercial milk supplies. Additionally, the USDA had mandated testing of all dairy cattle prior to interstate travel beginning April 24, 2024. With regard to avian infections, the USDA Animal and Plant Health Inspection Services (APHIS) is conducting surveillance in captive wild birds across the country. However, because this is being done using captured birds at rehabilitation centers that may already be sick or need human assistance, this data may not be wholly representative of active influenza strains circulating in live, wild birds. Additionally, while data from infected bird mortality is useful for tracking highly pathogenic bird strains, it does not necessarily capture other strains that might be undergoing mutation and showing reduced pathogenicity in birds. Mapping the prevalence of these strains is incredibly important for understanding how the virus is evolving, since reduced infection in birds could mean that the virus can more easily jump into other species.
You may be wondering why additional animal infection surveillance is not being done. For starters, it’s expensive. In May, the U.S. Department of Health and Human Services announced a $101 million budget through the CDC and FDA for monitoring avian influenza with a goal to keep communities informed, ensure the safety of the food supply, protect agriculture and farmers, and monitor influenza trends to mitigate the risk to humans. The CDC contributed an additional $93 million to support testing and laboratory functions, epidemiology and surveillance efforts, and vaccine development. Because avian influenza has cropped up across the country, however, monitoring and managing viral spread requires high levels of coordination between numerous organizations.
Federal agencies are not the only entities contributing to viral surveillance who depend on government funding, either. Recently, the U.S. government has halted funding for other organizations, such as the viral surveillance organization EcoHealth Alliance. Following controversy surrounding the COVID-19 pandemic, which involved an alleged failure to comply with the terms set forth by their grant, the government suspended their funding this past May. While this piece will not focus on the controversy surrounding COVID-19, it is important to note that this organization was also monitoring other threatening viruses, such as the highly lethal Nipah virus and avian influenza. Among the debate surrounding EcoHealth’s halted funds, worries are also rising about whether this suspension will possibly disincentivize viral surveillance efforts, which require millions in government funding to operate. Issues with funding have already been observed at the state level; a recently passed California budget aiming to reduce budget deficits by $16 million via spending cuts could raise issues when it comes to monitoring transmission of viruses like avian influenza through wastewater.
Conclusion
For now, the CDC still considers H5N1 avian influenza a low risk to humans. Continued surveillance efforts across species including birds, cattle, and humans will be necessary to monitor the situation. However, avian influenza will not simply disappear if government funding for surveillance runs out. Viruses are persistent and can crop up unexpectedly, characteristics that prove difficult for viral management and monitoring. To stay ahead of possible epidemics, surveillance organizations must have the funding and direction needed to keep tabs on viruses as they spill over and evolve. The COVID-19 pandemic saw a boom in research funding to groups studying viruses, but as the pandemic has started to gradually wind down, the number of coronavirus research grants awarded has fallen. The number of influenza grants awarded by the NIH has been steadily increasing from 2008, but it is important that viral research funding continues to be supported, especially when it comes to hunting for novel viruses and supporting infrastructure to deal with emerging epidemics.

It’s also important to be aware of avian influenza spread occurring outside of the U.S. So far, there have been 8 human cases of H5N1 in the Western Pacific region this year, with two deaths in Cambodia and Vietnam. Comprehensive epidemic and pandemic preparedness involves the whole world, and other countries have famously not received the same opportunities to monitor viral disease. Recent attempts to ameliorate this disparity, such as the WHO’s Pandemic Treaty, have also faced significant challenges. As humanity continues to spread further into wild land, particularly into tropical regions with high biodiversity, we will encounter more unknown diseases. Rising temperatures associated with climate change are also predicted to force animals out of their usual habitats and into our spaces, thus increasing opportunities for contact and spillover into humans. In fact, it’s already happening, as evidenced by the increase in dengue cases popping up across the United States due to an expansion in the habitat range of virus-carrying mosquitoes.
While avian influenza may not necessarily be the next major pandemic, these recent outbreaks—in addition to decreased funding for virus surveillance—have revealed just how underprepared we may be. Protection against disease doesn’t just occur at the individual level; it requires collaboration at the global level. If we want to be better prepared for the next pandemic, we need international cooperation as well as support for pandemic preparedness and research into viruses with pandemic potential.





I'm a med student and this was incredibly easy to understand, thank you so much for this!